GASTROSCOPY
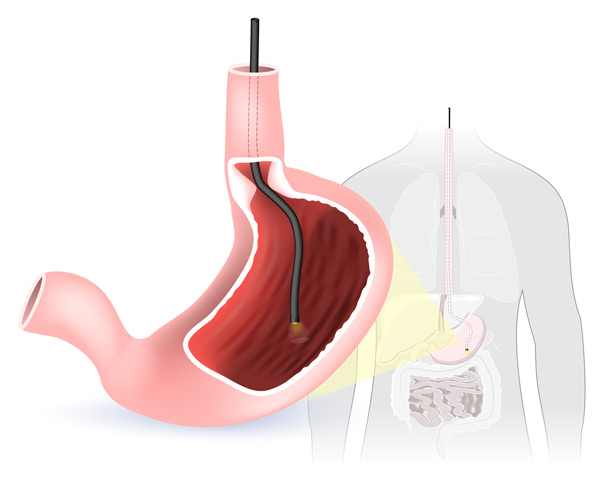
ABOUT THE PROCEDURE
- During a gastroscopy, a thin flexible tube is used to examine the oesophagus (gullet), stomach and duodenum (top part of the small intestine)
- The test takes approximately 10 minutes to perform
- Common reasons to have a gastroscopy include the investigation of heartburn or reflux symptoms, upper abdominal pain, swallowing difficulties, anaemia, possible internal bleeding and to diagnose coeliac disease
- Biopsies or small samples of the oesophagus, stomach or duodenum may be taken during the gastroscopy to assist with diagnosis and exclude bacterial infections such as Helicobacter pylori
RISKS AND COMPLICATIONS
- Gastroscopy is a safe procedure with serious risks such as bleeding or perforation being described in less than 1 in 10,000 procedures
- A sore throat may occur after the procedure
FASTING INSTRUCTIONS
South Perth hospital St John of God Murdoch Hospital
COLONOSCOPY
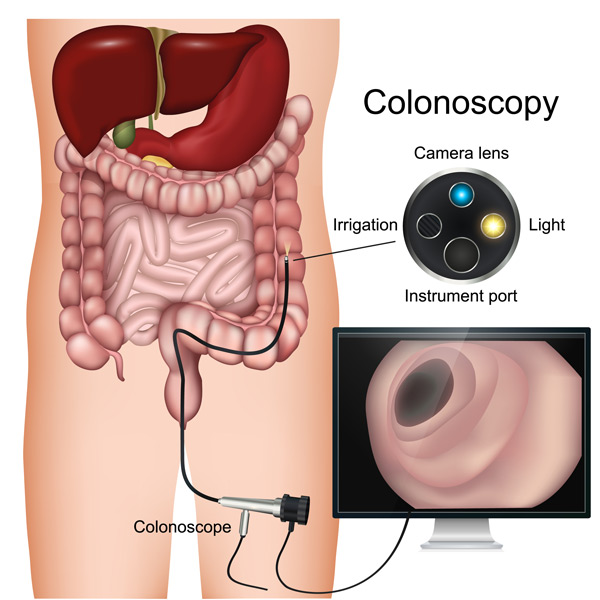
ABOUT THE PROCEDURE
- During a colonoscopy, a thin flexible tube is used to examine the colon (large intestine) and ileum (lower part of the small intestine)
- The test takes approximately 20-30 minutes to perform
- Common reasons to have a colonoscopy include the investigation of rectal bleeding, alteration in bowel habits, positive stool blood test, anaemia and abdominal pain. You may also be recommended to have a colonoscopy as a bowel cancer screening test or surveillance test if you have a family or personal history of bowel cancer or polyps.
- Bowel cancer usually arises from small growths in the colon called polyps
- If any polyps are detected they are usually removed during the colonoscopy to reduce future development of bowel cancer
- Biopsies or small samples of the colon may be taken during the colonoscopy to assist with diagnosis
RISKS AND COMPLICATIONS
- Colonoscopy is a safe procedure with serious risks such as bleeding or perforation (a puncture of the intestine) being described in less than 1 in 1000 procedures
- A few patients report abdominal discomfort or bloating after the procedure which usually abates within a few hours
PREPARATION AND FASTING INSTRUCTIONS
- The bowel preparation is extremely important and commences 2 days prior to the procedure
- South Perth Hospital
- St John of God Murdoch Hospital
INFORMATION FOR ALL PROCEDURES
MEDICATIONS
- Please advise us if you take clopidogrel (Plavix), warfarin or other blood thinning medications as these may need to be stopped before the procedure
- If you take iron tablets please stop them at least 1 week before the procedure
- If you are diabetic and take Forxiga (dapagliflozin) or Qtern (saxagliptin + dapagliflozin) or Xigduo (dapagliflozin + metformin) you must stop these medications 3 days prior to your colonoscopy.
ANAESTHETIC
- As the procedure can be an uncomfortable test, you will be given a light anaesthetic by an anaesthetist. This involves an injection of sedative medication into a vein in your arm or hand. You will have little or no recollection of the test.
PRE-PROCEDURE CONSULTATION
- You will meet me and your anaesthetist immediately prior to your procedure.
- You will have the opportunity to discuss your symptoms, the procedure and the anaesthetic with us. You will then be asked to sign a consent form for the procedure.
PREPARATION FOR THE PROCEDURE
- If you are having a gastroscopy only, make sure you carefully follow the fasting instructions provided to you
- If you are having a colonoscopy make sure you carefully follow the bowel preparation and fasting instructions provided to you
- Please ensure you have someone to take you to the hospital and pick you up after the procedure. You will not be allowed to drive for 12 hours due to the anaesthetic
FOLLOWING THE PROCEDURE
- After the procedure and after you have woken up from the anaesthetic you will be offered something to eat and drink
- Results and follow up will be explained to you and you will be given a written report for your own records
- It is recommended to make an appointment with your GP within 2 weeks of your procedure to get the results of any biopsies and discuss ongoing management
QUESTIONS AND CONCERNS ABOUT THE PROCEDURE
- If you have further questions or concerns regarding your procedure please contact me or your GP prior to the procedure
- If you develop pain or significant bleeding after the procedure please contact me during office hours or attend your nearest hospital emergency department
CONSULTATIONS
Your initial consultation will involve the taking of a full medical history, a physical examination and a plan for investigation and ongoing management of your gastrointestinal condition. It may take up to 45 minutes. Please bring with you a full list of your medications, any X-rays, scans and relevant blood test results as well as your GP referral letter/form.
With your consent, all of our communication with you will be via email, telephone and text message (appointment reminders only).
If you are elderly or frail or have multiple complex medical problems or severe lung or heart problems, you may require a consultation prior to any endoscopic procedures. This will allow full discussion of the risks and benefits of these procedures and will ensure your medical conditions are optimised pre-procedure.
If you are uncertain about whether you need a consultation prior to any endoscopic procedure we suggest you discuss this with your GP or contact my consulting rooms.